Restless and struggle to focus? A never-ending to-do list that never seem to be completed? Yeah, I’ve been there. Quite honestly, it has become increasingly difficult to sit still and focus on only one thing at a time – especially with the gradual technology “improvements,” latest news updates, and all the “social media experts” giving mental health advice. But is it ADHD?
ADHD has received more attention recently and rightfully so – many have gone far too long with undiagnosed symptoms and support. Have you ever wondered if your difficulty focusing, restlessness, or emotional overwhelm is really ADHD? Or maybe something else?
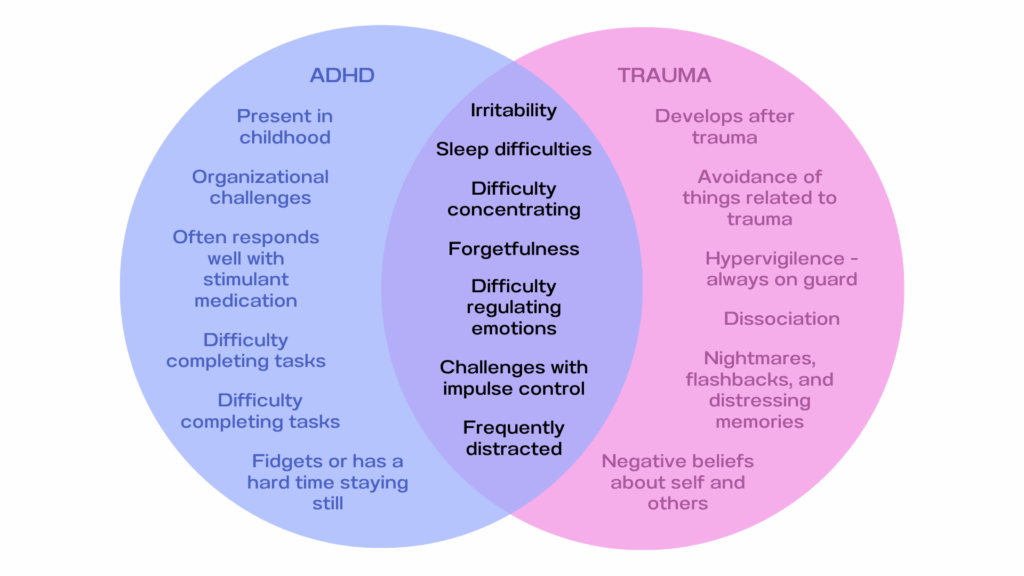
Even as there is more awareness and discussion about ADHD, its overlap with reactions to trauma is often left out or underrepresented in those same talks and social media posts. The truth is, ADHD is often over diagnosed in individuals with trauma histories when trauma responses may be masked as ADHD symptoms. As a trauma-informed therapist, I work with many clients who relate to both ADHD traits and symptoms of unresolved trauma. While they are not the same, there are some striking familiarities between the two experiences.
So, What Really is ADHD?
ADHD stands for Attention-Deficit/Hyperactivity Disorder. This name has medically replaced the older acronym “ADD.” According to the DSM-5-TR, the diagnosing manual for mental health professionals, ADHD is defined as a “neurodevelopmental disorder characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development.” It commonly includes the following symptoms:
- Easily distracted by extraneous stimuli
- Forgetfulness in daily activities
- Struggles in time management
- Difficulty sustaining attention
- Fidgets with or taps hands or feet, or squirms in seat
- Restlessness
- Impulsivity
ADHD is not caused by trauma – however, trauma can worsen ADHD symptoms, or even mimic them entirely.
So, What Really is Trauma?
Trauma is how the body and brain respond to an experienced event that overwhelms your ability to cope. It is not necessarily the event itself and can also be the accumulation of multiple experiences. While trauma is often thought of as a single life/safety-threatening event such as a car accident, trauma can also be caused by more chronic situations such as systemic oppression, racism, military experiences, and abuse. Such experiences can negatively affect your nervous system’s sense of safety. As a result, developed symptoms can affect multiple facets of daily functioning that persist well after the conclusion of the traumatic incident itself. Aspects that can be affected by trauma are:
- Attention
- Memory
- Emotional regulation
- Mood
- Sleep/energy levels
- Trust in self and others
- Body awareness and sensitivity
When someone experiences a trauma, or chronic, repeated traumas, they may develop a trauma-related disorder such as posttraumatic stress disorder (PTSD).
So, What is the Overlap Between ADHD and Trauma?
Both symptoms of ADHD and unresolved trauma can lead to:
- Difficulty concentrating
- Irritability
- Zoning out
- Restlessness
- Impulsivity
- Sensory sensitivities
- Trouble with follow through
- Difficulty managing emotions
From the outside, and even the inside too – it can be difficult to dissect exactly what is the cause of each symptom. Misdiagnosing is common, especially among professionals who are not trained in trauma-informed approaches. The diagram below is not a comprehensive list of symptoms, but gives an overview of some of the similarities and differences between ADHD and trauma-related symptoms.
A Deeper Dive
The brain and body are connected more than most realize. The body’s innate goal is to keep us safe. When an individual’s safety has been threatened during multiple experiences and/or one life-defining experience, the body adapts by staying on alert. It’s not that an individual necessarily likes being hypervigilant, but it is the body’s way of avoiding additional threats. Think of it as a bodyguard, whose job is so important they cannot risk taking breaks to rest. The constant vigilance though, can look a lot like the hyperactivity or distractibility we see in ADHD.
For example:
- A trauma survivor may appear inattentive because they’re constantly scanning for danger
- An individual’s impulses may be difficult to control because their nervous system is focused on the now, not later
- A survivor may have unpredictable emotional outbursts as they are overwhelmed by the need to regulate current emotions alongside unprocessed (and often repressed) emotions related to the trauma
This is why trauma-informed care is so important. Rather than asking “What’s wrong with you?” we ask, “What happened to you?”
ADHD, Trauma, or Both?
It is possible, and quite common, to have both ADHD and unprocessed trauma. Here, symptoms may be heightened and more difficult to manage without adequate knowledge and support. Resulting tension in the body can further lead to physical disruptions such as chronic pain, migraines, IBS, loss of appetite or emotional eating, hormonal imbalances, and autoimmune flare-ups further making symptom management difficult.
How Therapy Can Help
If you’re unsure about the cause of your symptoms and/or how to manage them, consider seeking support from a licensed mental health professional. A licensed therapist or psychiatrist who has been trained in trauma can support you by providing a comprehensive assessment that allows for a deeper exploration of symptoms. A trauma-informed lens ensures that factors are not overlooked and increases your partnership in an individualized plan towards healing.
At TREC DC, we offer integrative care that supports your whole self – mental, physical, spiritual, and emotional. Our work together may include:
- Comprehensive psychological assessment
- Skills to regulate your nervous system
- EMDR therapy for trauma resolution
- Somatic practices to reconnect with your body
- ADHD-friendly strategies for executive function and focus
- Emotional processing in a safe, compassionate space
You don’t have to figure this out alone.
Trauma and ADHD are both real, valid experiences – and sometimes they co-exist. Understanding the overlap is not just about getting the right diagnosis; it’s about receiving the kind of care that honors your full story.
If you’re ready to explore your symptoms through a trauma-informed lens, I invite you to reach out. Your healing is possible.